Canada’s Experience with Covid-19 and CAMH
How Child and Adolescent Psychiatry has changed in Toronto Post COVID-19
By Raj Rasasingham M.D.FRCPC.DAPN., Section Chair, Global Psychiatry, Canadian Academy of Child Psychiatry, Head of Outpatient Child Psychiatry, HRH, University of Toronto
COVID-19 has had a significant impact around the world in the way we practice medicine. Child Psychiatry has changed significantly as well. Virtual care is now standard for most hospitals and private practices in the Toronto Region. Walk-In Children’s Mental Health clinics have been converted into telephone/virtual walk in clinics around the Toronto region. The number of inpatient beds has been reduced in the system since some have been redeployed to make room for COVID-19 units. However, the child psychiatry community has gotten closer and worked together to solve these problems. We have regular meeting at all levels to work together and share ideas on how we can move forward and manage the crisis.
The end result is that the clinicians are still providing quality care to our patients and families. Many are working from home, mostly virtually, but they are still providing quality care to their patients and families. Our team meetings and case conferences are thorough the virtual medium. There are safety and social distance protocols in every hospital and community mental health centre in the region.
Academic teaching and conferences are still happening but we are doing it via the virtual medium. I am truly amazed by the creativity of our teachers and learners.
We have adapted to the new reality, but the end result may be more comprehensive care to the patients and families we serve. Most have found the crisis an opportunity to embrace technology and expand the scope of their practice.
Covid 19 and Child and Adolescent Services in Calgary Canada
By Chris Wilkes, B.Sc., M.B., ChB., M. Phil. D.C.H., F.R.C.P. (Edin), F.R.C. Psych., F.R.C.P.(C), D.L.F.A.P.A., I.A.A.P., Professor, University of Calgary, Division Head, Child and Adolescent Psychiatry, Alberta Health Services & University of Calgary
So far Calgary and Alberta have survived the Covid-19 pandemic relatively well with approximately 7000 cases and 150 deaths. However, the Covid shut down had a dramatic impact on our child and adolescent services and on us personally. This included the dramatic closure of our schools and closing down of two of our adolescent units, day programs and changing all of our outpatient’s services to virtual services with Zoom or phone. Now most patients have adapted to the convenience of virtual assessments quite well, even though this transition means some of the psycho-metrics need to be booked later, when the lock down is over and we have relaunched outpatient visits. But the major impact was on families who have to do home schooling and also work from home. Our hospitals, ER services and outpatient services were eerily quiet.

Empty hospital corridors
Cuddly toys with masks
Additionally, there has been a sudden decrease in workload for our inpatient psychiatrists resulting in a massive re-deployment to outpatient services and online support programs for families. The stress of the COVID 19 pandemic certainly affects all of the mental health professionals, allied professionals, and families in many different ways. We noticed that many patients with anxiety disorders enjoyed staying away from school at first before boredom and isolation set in. Those with depression struggled with no routine and reduced opportunities for behavioral activation. All playing fields and parks were off limits. Making online contact with support staff, therapist and doctors even more essential.
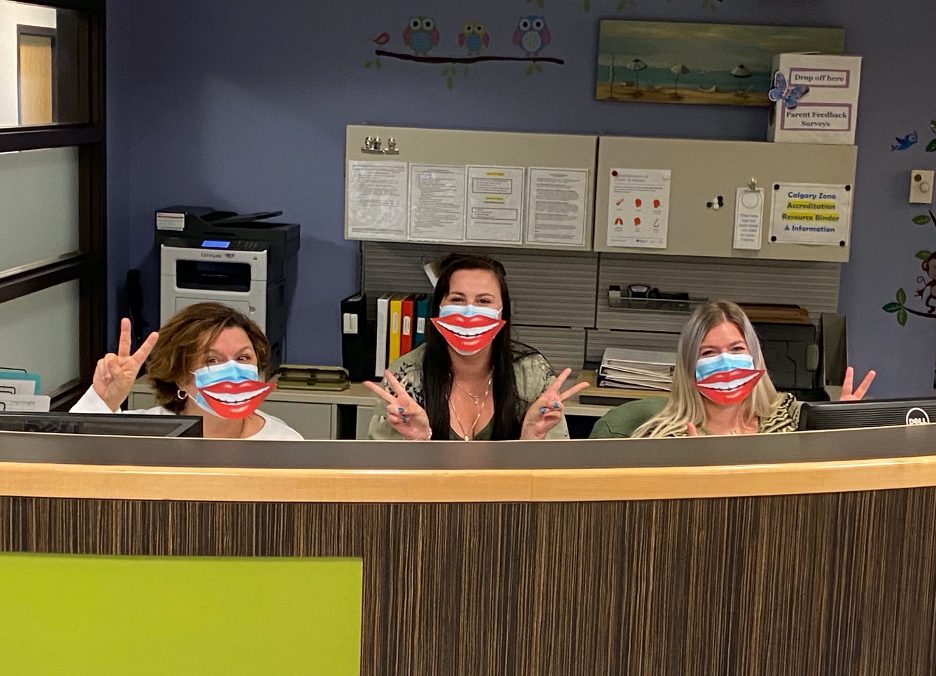
Friendly staff

Online meetings become the new norm
Personally speaking, this can be both an anxious and depressing time when our schedules and workloads are constantly changing. Trying to provide in home support to children and grandchildren due to the schools and day care centers being closed is very unsettling and a challenge. Of course our restricted mobility is also a challenge as we have to rely on virtual information and here say rather running around the city doing multiple consults in a variety of settings. Resulting in new fears of missing information or doing incomplete assessments. Unfortunately teaching via Zoom can be a major challenge as well due to the logistic problems such as “Sorry I can’t hear you, or your video has frozen in and out” resulting in a new DSM 5 condition called Zoom fatigue and loss of the usual rewards we all feel with direct patient and student encounters. But at last we can see the light at the end of the tunnel as we prepare for re-launching services and reconnection with patients and colleagues around June 22nd. Yet our confidence that life will return to normal is challenged by the fact we have to learn to live with the COVID 19 threat. Life will never be quite the same and now we all trying to be more mindful and find meaning, radical acceptance and gratitude with our new reality.

Dr Chris Wilkes and colleagues on a Zoom meeting